New Horizon Family Health Services serves all patients regardless of ability to pay. However, services are not provided free of charge.
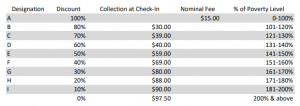
New Horizon Family Health Services is a Federally Qualified Health Center (FQHC) and receives some federal funding to help offset the cost of providing care to patients on a sliding fee scale. Eligibility for the sliding fee discount is determined by documented annual income and family/household size. Patients with a documented annual income of 200% or below the federal poverty level (FPL) are eligible for a sliding fee discount on all services we provide, including prescriptions written by New Horizon Family Health Services providers and filled at New Horizon Family Health Services pharmacies.
Patients with income at or below 100% of the federal poverty level (FPL) are charged a nominal fee; however, no established patient will be refused services due to inability to pay. Patients unable to pay the discounted fee at the time of service will be required to sign a payment plan agreement.
Determining your eligibility for the sliding fee discount requires verification of your income. This information must be updated at least annually to continue your participation in the program. This information is only used to calculate your discount and is kept completely confidential.
Sliding fee discounts for essential services are offered based upon family size and income. Proof of income is required. You may apply for sliding-fee discount at the front desk.
How do I qualify?
If you wish to apply for the Sliding Fee Discount you MUST show proof of gross annual income for all immediate family members living in your household. Gross income is ALL income from ALL sources before taxes.
Acceptable Income Documentation for Sliding Fee Application Includes:
Self-Declaration of Income Form:
There may be some circumstances when it is important that a patient be seen but does not have income documentation during their visit. A patient may apply using a self-declaration form.
New or established patients can use a self-declaration form. Patients can use the self-declaration from one time in a rolling calendar year. The sliding fee designation expires after 10 days and on day 11, if the patient does not have sufficient income documents, he/she will be self-pay with no discount on the services rendered.
Collection at Check-In:
For patients with insurance, the insurance is the Primary Payor Source. Collect the required co-pay as outlined by insurance plan. If the patient has both insurance and sliding fee the lower amount should be collected.
Patients with sliding fee only: Use the following table as a guide to collect point of service payment. If you do not collect the full amount, make a note. The collection or nominal fee at check-in is a payment toward patient responsibility. Established patient collection is $80.00 and new patient collection is $97.50.